Managing Diabetes: Diagnosis, Monitoring & Understanding with GlucoRx
01/11/2025
Nearly 6 million people in the UK are living with and managing diabetes, including over a million who remain undiagnosed.
Introduction
Every practice day brings the same rhythm. Routine checks, quiet conversations, results that shape months of care. Managing diabetes isn’t rare, and yet each case feels personal. Behind every reading is a life being balanced between medication, meals, movement, and mindset. The role of the clinical team is to translate numbers into understanding and give patients confidence in their control.
What Is Diabetes?
Diabetes is a chronic condition where the body struggles to regulate glucose. Insulin, the hormone that moves sugar into cells for energy, is either absent, insufficient, or resisted. The result is persistent high blood sugar (hyperglycaemia) which, if unmanaged, can damage vessels, nerves, and organs over time.
The four key forms of diabetes include:
• Type 1 Diabetes: Autoimmune destruction of pancreatic beta cells; complete insulin deficiency.
• Type 2 Diabetes: Insulin resistance combined with gradual loss of secretion.
• Gestational Diabetes: Temporary insulin resistance during pregnancy.
• Prediabetes: A metabolic warning stage where glucose levels are high but not yet diabetic.
Each type differs in cause and progression, but shares a single clinical aim: maintain glucose control to prevent complications.
Diabetes Causes and Risk Factors
The roots of diabetes extend beyond diet.
Genetics, excess weight, sedentary behaviour, and pancreatic function all play a part. For Type 2 especially, prevention hinges on lifestyle modification.
Modest weight loss and regular physical activity can delay or halt progression.
Risk-assessment tools, such as the Diabetes UK Risk Score, allow practices to identify patients early. A short form, a few quick questions, and patterns begin to appear. Age, waist circumference, family history, etc.
Each answer refines the picture of who might benefit from screening before symptoms arise.
Recognising the Symptoms of Diabetes
Diagnosis rarely starts with a headline symptom.
It’s the everyday complaints that draw attention:
• Increased thirst and urination
• Fatigue
• Blurred vision
• Slow wound healing
For clinicians, these signs are subtle prompts to investigate further rather than conclude.
Early detection can help prevent progression, and reduces the long-term burden on both patient and practice.
Those early clues often guide what comes next.
GlucoRx
Supporting Better Diabetes Management with GlucoRx
Diagnosing Diabetes in Primary Care
Diagnosing diabetes begins long before a lab result.
Often, it’s in the subtle clues, including the symptoms in the previous section. From there, the process becomes a matter of measurement and confirmation.
Key diagnostic tools include:
• HbA1c test: the gold-standard for long-term glucose trends.
• Fasting plasma glucose: snapshot of baseline control.
• Oral glucose tolerance test: how the body responds to glucose load.
• Self-monitoring of blood glucose: supports day-to-day understanding and adjustment.
Each result gives a piece of the picture. Together, they define the patient’s path.
From prediabetes (42–47 mmol/mol) to Type 2 diabetes (48 mmol/mol and above).
Imagine that a patient’s home readings were logged using a GlucoRx meter, and the readings automatically synced to your practice system. The data revealed a gradual morning spike the patient hadn’t noticed. A small medication adjustment, guided by real numbers, brought the next HbA1c down. Quietly and effectively.
That’s the kind of clarity that accurate diagnosis and monitoring delivers.
Treatment and Ongoing Diabetes Management
Once diagnosed, management can be a part of your patient’s routine:
• Lifestyle: balanced diet, controlled carbohydrates, regular movement.
• Medication: metformin, GLP-1 agonists, SGLT2 inhibitors, or insulin depending on type and response.
• Monitoring: frequent glucose checks and periodic HbA1c testing.
Consistency can change outcomes.
A nurse adjusting insulin doses reviews logged readings between appointments. Stable morning averages could mean fewer phone calls, and fewer worries. Just steady, evidence-based control.
Monitoring Equipment and Technology
Technology can now support every part of this process.
Modern glucose meters, continuous monitors, and mobile apps reduce barriers to self-care and data sharing. During routine reviews, practices using GlucoRx Connect could notice fewer gaps in patient logs. Results upload automatically, trends appear instantly, and both clinician and patient see progress in real time.
No fuss. Just the assured reliability that lets conversations focus on lifestyle, and not missing numbers.
Reliable readings lead to reliable decisions. That’s the practical value of well-designed equipment in everyday primary care.
Preventing Long-Term Complications
Good control protects more than glucose levels.
It reduces risk of:
• Neuropathy: nerve damage causing pain or numbness.
• Retinopathy: eye damage detected through annual screening.
• Nephropathy: kidney impairment monitored via urine ACR and eGFR.
• Cardiovascular disease: Target blood pressure guided by NICE. <140/90 mmHg for most adults under 80, and <130/80 mmHg for those with diabetic kidney disease.
Each small improvement can accumulate over time, leading to years of enhanced patient lifestyle and greater independence.
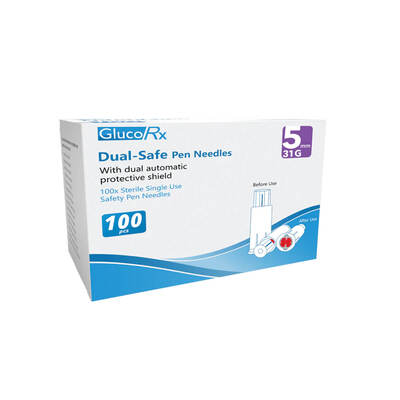
Clinical Care and Infection Control
Routine care also depends on safe practice.
Consumables like single-use lancets, sharps containers, and clinical-waste segregation protect both staff and patients.
Every disposal and decontamination step needs to align with NHS infection-prevention guidance.
Compliance isn’t bureaucracy. It’s the basics of patient safety.
GlucoRx Consumables
Trusted GlucoRx Consumables for Managing Diabetes
Nutrition and Lifestyle Support for Managing Diabetes
Education underpins every management plan.
The NHS Diet for Type 2 Diabetes encourages portion control, higher-fibre foods, and reduced refined carbohydrates.
Carbohydrate counting helps insulin users match dose to intake. Exercise improves insulin sensitivity and cardiovascular health. Here too, technology assists.
A dietitian reviewing a patient’s GlucoRx log might see post-meal peaks flatten over time. Visible proof that dietary advice has landed.
Guidelines and Trusted Authorities
Best practice remains grounded in evidence.
Clinicians follow frameworks from NHS, NICE, WHO, and Diabetes UK.
These define diagnostic thresholds, treatment algorithms, and monitoring intervals. Ensuring every decision aligns with recognised standards.
Conclusion
Diabetes management is built on precision, patience, and partnership.
Accurate readings, clear targets, and small adjustments compound into long-term stability.
Tools like GlucoRx support that process. Not by transforming care overnight, but by making everyday accuracy effortless.
When patients and clinicians see the same reliable data, trust follows naturally.
Next Steps for Managing Diabetes
Review your current diabetes-monitoring setup. Explore the GlucoRx range available at Williams Medical Supplies. Validated and NHS-approved devices designed for clarity, consistency, and confidence in primary-care practice.
About Williams Medical Supplies
Williams Medical Supplies helps healthcare professionals deliver safer, more efficient, and compliant care through trusted products and reliable support every day.
Resources
Services to help you manage diabetes.
Official NHS information on diabetes symptoms, treatment, and ongoing care, designed to support both patients and healthcare professionals with evidence-based guidance.
Comprehensive clinical recommendations and best-practice standards from the National Institute for Health and Care Excellence (NICE), including diagnostic thresholds and management frameworks.
The UK’s leading diabetes charity offering patient resources, professional education, and up-to-date statistics on the national impact of diabetes.
A trusted UK manufacturer of blood-glucose monitoring systems and diabetes-care technology used across NHS primary and secondary care.
Disclaimer: This article is intended for educational and informational purposes only and is not a substitute for professional medical or clinical advice. Healthcare professionals should always use their own clinical judgment, follow local governance procedures, and consult current NHS and NICE guidelines when making patient-care decisions. Patients should seek guidance from a qualified healthcare provider regarding diagnosis or treatment of any medical condition.